Mending Broken Hearts
Cheeseburgers, smoking, stress, the rise of the couch potato: These are the usual suspects on the list of risk factors for heart disease, a malady reaching global epidemic proportions. Now discoveries about genetic triggers may help us spot trouble before it starts.
Gloria Stevens is lying on her back, sedated but alert, staring at an image of her own beating heart. Metaphorically, Gloria’s heart is the very core of her emotional self—not to be worn on the sleeve, much less displayed on an overhead monitor. More literally, it is a blood-filled pump about the size of a clenched fist whose rhythmic contractions have kept Gloria alive for 62 years, and with a little tinkering will keep her going for an indeterminate number more.
At this moment, her doctor is threading a thin catheter up through her femoral artery from an incision in her groin, on into the aorta, and from there into one of the arteries encircling Gloria’s heart. At the tip of the catheter is a small balloon. The doctor gently navigates the tip to a spot where plaque has narrowed the artery’s channel by 90 percent. With a quick, practiced movement he inflates the balloon to push back the artery wall, deflates the balloon, then inserts an expandable stent—it looks like a tiny tube of chicken wire—that will keep the passage open. As Gloria watches on the monitor, the crimp in her artery disappears, and a wide laminar flow gushes through the vessel, like a river in flood.
The procedure is over. It has lasted only half an hour. In all likelihood, Gloria will be able to go home the next day. So will a few thousand other patients in the United States undergoing such routine angioplasty—more than a million of them a year. Pipe fixed, patient cured, right?
Wrong.
Because of her treatment, Gloria’s quality of life will likely improve. She’ll breathe easier and maybe live longer. But she is hardly cured. Her coronary atherosclerosis—a hardening and narrowing of the arteries that supply the heart with oxygen-rich blood—still leaves her vulnerable to future blockages and coronary heart disease.
Although hearts suffer many maladies—valves leak, membranes become inflamed—coronary heart disease, which can lead to heart attack and ultimately to heart failure, is the number one killer of both men and women in the United States, where 500,000 die annually. Worldwide, it kills 7.2 million people every year. Exacerbated by the export of Western lifestyle—motorized transport, abundant meat and cheese, workdays conducted from the comfort of a well-padded chair—incidence of the disease is soaring.
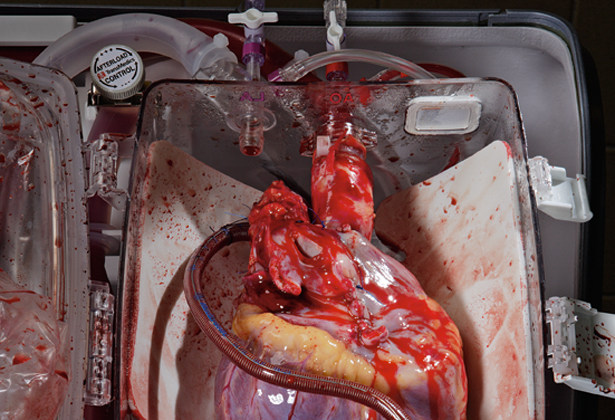
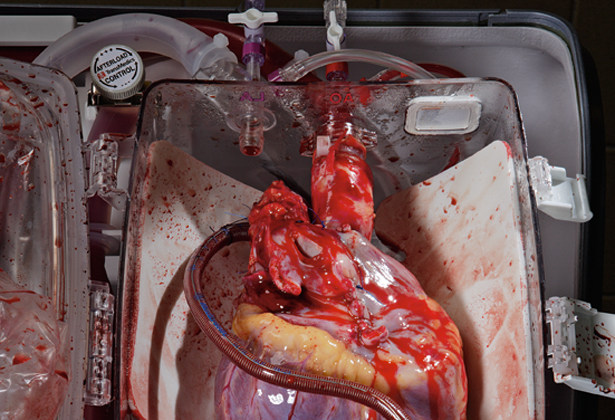
To help stem this lethal tide, cardiologists can prescribe such cholesterol-lowering drugs as statins to help keep arteries clear. They can advise patients to change their habits, or they can operate to fix an immediate problem. Angioplasty is one procedure, and surgery to bypass the diseased arteries is another—each year more than 400,000 bypasses are performed in the U.S. Transplants can replace severely damaged hearts, and artificial ones can keep people alive while they wait for a donor heart. But in the face of an impending global epidemic, none of these stopgap measures addresses the essential question: Who gets heart attacks and why?
The human heart beats 100,000 times a day, propelling six quarts of blood through 60,000 miles (97,000 kilometers) of vessels—20 times the distance across the U.S. from coast to coast. The blood flows briskly, surging out of a ten-ounce (0.3 kilograms) heart so forcefully that large arteries, when severed, can send a jet of blood several feet into the air. Normally the relentless current helps keep blood vessels clean. But where an artery bends, tiny eddies form, as in a bend in a river. This is where bits of sticky, waxy cholesterol and fat can seep into the artery wall and oxidize, like butter going rancid. Other matter piles up too. Eventually, the whole mass calcifies into a kind of arterial stucco, or plaque.
Until recently, cardiologists approached heart disease as a plumbing problem. Just as mineral deposits restrict the flow of water through a pipe, an accretion of plaque impedes the flow of blood through an arterial channel. The more crud in the system, the greater likelihood that a dammed artery will trigger a heart attack. Doctors now dismiss this “clogged-pipes model” as an idea whose time has passed. It’s just not that simple.
Most heart attacks are caused by plaque embedded within the artery wall that ruptures, cracking the wall and triggering the formation of a blood clot. The clot blocks the flow of blood to the heart muscle, which can die from lack of oxygen and nutrients. Suddenly, the pump stops pumping.
Contrary to the clogged pipes model, heart attacks generally occur in arteries that have minimal or moderate blockage, and their occurrence depends more on the kind of plaque than on the quantity. Scientists have been struggling to figure out what type is most responsible. Paradoxically, findings suggest that immature, softer plaques rich in cholesterol are more unstable and likely to rupture than the hard, calcified, dense plaques that extensively narrow the artery channel. But understanding the root cause of the disease will require much more research. For one thing, human hearts, unlike plumbing fixtures, are not stamped from a mold. Like the rest of our body parts, they are products of our genes.
Don Steffensen was putting duck-hunting decoys out on a small lake one fall afternoon in southwestern Iowa when his heart attack hit. The infarction was massive and unexpected. It’s likely that Steffensen survived only because a buddy was carrying nitroglycerin tablets and quickly slipped one under his friend’s tongue. Nitroglycerin is used to make dynamite; in the body, a heavily diluted form releases nitric oxide, which signals the smooth muscle cells in veins and arteries to relax, dilating the vessels.
The Steffensen clan is enormous: more than 200 relatives spread over three generations, many of the youngest are now dispersed from Iowa to New York and beyond. Although heart trouble is common in the family, it had never struck anyone as unusual. “I attributed it to diet,” shrugs Tina, a slim 38-year-old and the family’s only vegetarian.
It was a reasonable conclusion. The Steffensens were raised on the kind of farm food that the state is famous for—ham balls, meatloaf, pie, macaroni and cheese—and still popular even as careers have moved indoors. Driving north through cornfields to meet some of the family in Buffalo Center, I dined at a restaurant offering deep-fried sandwiches. A single ham and cheese hoagie—dunked in hot fat and served sizzling—seemed capable of stopping a heart all on its own.
But could the high incidence of heart trouble among the Steffensens be related to something else besides high-fat diets? Eleven years after Don’s attack, his wife, Barbara, happened to overhear a doctor describing a study about the genetics of heart attacks.
Curious, Don and 20 of his relatives each sent a vial of blood to the Cleveland Clinic, where the research was being conducted. Eric Topol, a cardiologist and genetics researcher at the clinic, spent a year studying their DNA. Each person’s genome comes with millions of individual variations, but Topol was looking for something distinctive—and shared only by the members of the clan with heart trouble. The mutation he and his team finally spotted, in a gene called MEF2A, produced a faulty protein. “We knew we had something,” Topol says. “But the question was: How does this sick protein, present at birth, lead to heart attacks 50 years later in life?”
Topol himself is as lean as a greyhound and weathered in a cowboyish way. He talks slowly and eats minimally: salads for dinner and high-fiber cereal for breakfast. He doesn’t eat lunch at all. Like almost every cardiologist I’ve talked to, he takes statins preventively, and his cholesterol count is a low 135. His children, 22 and 25, also eat uncommonly well for their ages. “People have looked at the cadavers of men in their 20s who died in car accidents or as casualties of war, and nearly all had arterial cholesterol deposits,” Topol said as we walked to his lab. “This disease starts much earlier than people realize.”
Using endothelial cells (which line the inside of the artery wall) grown in culture, Topol set about figuring out what the MEF2A mutation does. He and his coworkers created some cells carrying the Steffensen variant, and others with the normal form of the protein. Both cell proteins were tagged fluorescent green so their locations could be visualized on a computer screen. The resulting images revealed a striking difference.
In a normal cell, all the MEF2A protein was inside the nucleus; on the screen, the cell resembled a fried egg with a fluorescent green yolk. But in the cells carrying the mutated version, the nucleus did not glow; instead the cell membrane was edged by a thin, luminous green line: a layer of MEF2A protein, trapped where it cannot serve its usual purpose. Topol believes that this defect affects the integrity of the coronary artery walls, rendering them more vulnerable to cracking when the plaque embedded in them ruptures. And each crack brings an increased chance of a heart attack.
Since this discovery, the Steffensens have become famous, appearing on shows like 60 Minutes II. Their mutant gene turns up in a Robin Cook novel titled Marker, about a health insurance company in New York that secretly screens patients for the MEF2A mutation and then kills them to preempt future medical-care payouts. Lively reading, but the Steffensen gene is an unlikely target for an insurance company, in part because it is an uncommon genetic defect.
Topol’s study did find that although dysfunctional MEF2A is very rare, the chance of heart disease in those carrying it may approach 100 percent. Most other genetic variations identified thus far increase the risk by much less. As it turns out, Topol himself carries a bum gene: apoE4, which affects inflammation in the arteries. Unlike MEF2A, it is common; every fourth person has it.
“Heart disease is not a one- or two-gene problem,” says Steven Ellis, a Cleveland Clinic cardiologist who oversees a 10,000-person genetic study known as GeneBank that collects DNA samples from patients who enter hospitals with atherosclerosis. Ellis, like most cardiac researchers, suspects that dozens of genes end up contributing to a predisposition: Some affect arterial integrity, others inflammation (which both causes and exacerbates arterial cracks), and still others the processing of lipids (the fats and cholesterol that turn into plaques). Of the several dozen genes, each may contribute just one percent to a person’s total risk—an amount that may be compounded, or offset, by outside factors like diet. As one doctor told me, any person’s heart attack risk is “50 percent genetic and 50 percent cheeseburger.”
The point of tracking down all these small mutations, Ellis explains, is to create a comprehensive blood test—one that could calculate a person’s genetic susceptibility by adding up the number of risky (and, eventually, beneficial) variables. Combined with other important factors, such as smoking, weight, blood pressure, and cholesterol levels, doctors could decide which patients need aggressive treatment, such as high-dose statins, and which ones are likely to benefit from exercise or other lifestyle changes. Some genes already can predict whose cholesterol level will respond strongly to dietary changes and whose won’t. Assessing risk is crucial, Ellis says, because heart disease is often invisible. In fact, 50 percent of men and 64 percent of women who die of heart disease die suddenly, without experiencing any previous symptoms.
Although standard tests can detect atherosclerosis, they aren’t foolproof. They may reveal plaques, but give no indication whether or not they are life-threatening. Tests like angiography, for example, where doctors inject a dye into the bloodstream and track it with x-rays, can show how much blood is flowing through an artery, but not discern the plaques embedded inside the artery wall—often the culprit in a heart attack.
Researchers have been working to solve this problem with scanners that provide pictures of the arterial wall itself, but it’s a tricky task. Normal cardiac artery walls are about a millimeter thick. Coronary arteries move with every beat of the heart, 70 times a minute. It’s tough to get a clear image of something so small in constant motion.
Difficult, but not impossible. As I walk through the basement of the Cleveland Clinic, I pass a room containing a large, blue, plastic doughnut as tall as I am, with a woman’s legs sticking out of the middle. The doughnut is a computed tomography (CT) scanner, a kind of three-dimensional x-ray machine that’s also used for imaging tumors. The scanner, aided by medications that reduce a patient’s heart rate and an injectable dye that highlights the arteries, can produce startlingly clear pictures.
Scrolling through images on his computer monitor, Mario Garcia, the clinic’s director of cardiac imaging, retrieves one that looks like a black-and-white landscape photographed from a plane, with a single, large river running through it. As Garcia zooms in on the river, a series of white lumps appears on the bank—hard plaques bright with calcium. But there is also a tiny black smudge. “That’s the type we believe causes a heart attack,” he says with satisfaction, pointing to the smudge of soft plaque. “It’s a rare opportunity to see that.”
As compelling as the CT scan is, it’s still an imperfect tool for predicting heart disease. It’s expensive, for one, and the dose of radiation from the x-rays makes it ill suited for use in healthy-patient annual exams. And although it sees arterial plaques, even soft plaques inside arterial walls, it can’t reveal whether those plaques are likely to crack and cause a heart attack.
Until there are tests, genetic or otherwise, that give a clearer measure of risk, everyone would be advised to exercise, watch their diet, and take statins for elevated cholesterol—the same advice doctors gave when the clogged-pipes model of heart disease reigned unchallenged.
At the Cleveland Clinic, cardiologist Stephen Nissen has conducted several studies on statins such as Lipitor, which reduce the amount of LDL (“bad” low-density lipoprotein) cholesterol made by the liver. Nissen is an advocate of lowering cholesterol by any means necessary. Does he take a statin? “You bet!” he says. “I have no intention of dying of the disease I treat.” His LDL level is a paltry 51. Of eight cardiologists I spoke with, all but one were taking the medication. (Some studies now seem to show that lowering even normal cholesterol levels has a protective effect.) HDL (“good” high-density lipoprotein) cholesterol is another story. Nissen calls it the “arterial-wall garbage barge” because of its ability to remove cholesterol from clogged arteries. Not all HDL can do this; some is dysfunctional. But tests have shown that raising the HDL level in genetically engineered lab mice can shrink their arterial plaques.