Curious, Don and 20 of his relatives each sent a vial of blood to the Cleveland Clinic, where the research was being conducted. Eric Topol, a cardiologist and genetics researcher at the clinic, spent a year studying their DNA. Each person’s genome comes with millions of individual variations, but Topol was looking for something distinctive—and shared only by the members of the clan with heart trouble. The mutation he and his team finally spotted, in a gene called MEF2A, produced a faulty protein. “We knew we had something,” Topol says. “But the question was: How does this sick protein, present at birth, lead to heart attacks 50 years later in life?”
Topol himself is as lean as a greyhound and weathered in a cowboyish way. He talks slowly and eats minimally: salads for dinner and high-fiber cereal for breakfast. He doesn’t eat lunch at all. Like almost every cardiologist I’ve talked to, he takes statins preventively, and his cholesterol count is a low 135. His children, 22 and 25, also eat uncommonly well for their ages. “People have looked at the cadavers of men in their 20s who died in car accidents or as casualties of war, and nearly all had arterial cholesterol deposits,” Topol said as we walked to his lab. “This disease starts much earlier than people realize.”
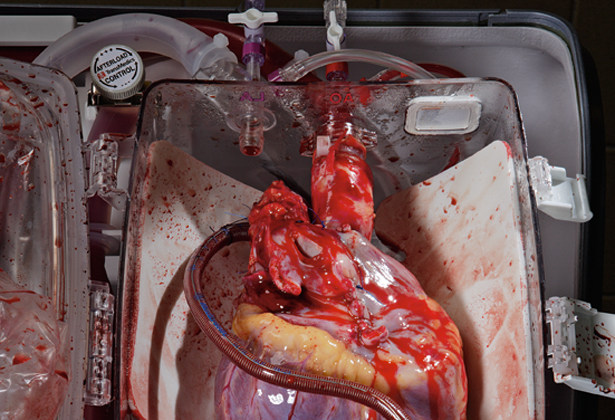
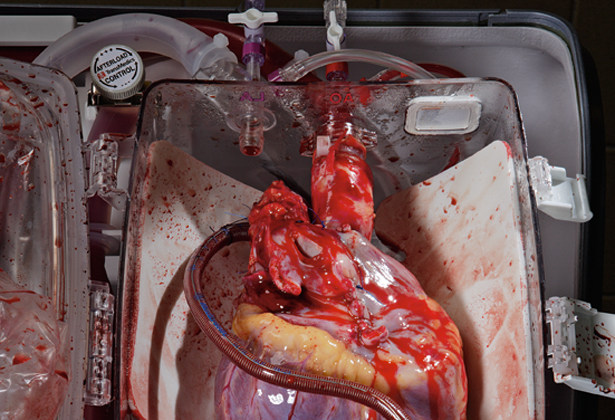
Using endothelial cells (which line the inside of the artery wall) grown in culture, Topol set about figuring out what the MEF2A mutation does. He and his coworkers created some cells carrying the Steffensen variant, and others with the normal form of the protein. Both cell proteins were tagged fluorescent green so their locations could be visualized on a computer screen. The resulting images revealed a striking difference.
Since this discovery, the Steffensens have become famous, appearing on shows like 60 Minutes II. Their mutant gene turns up in a Robin Cook novel titled Marker, about a health insurance company in New York that secretly screens patients for the MEF2A mutation and then kills them to preempt future medical-care payouts. Lively reading, but the Steffensen gene is an unlikely target for an insurance company, in part because it is an uncommon genetic defect.
Topol’s study did find that although dysfunctional MEF2A is very rare, the chance of heart disease in those carrying it may approach 100 percent. Most other genetic variations identified thus far increase the risk by much less. As it turns out, Topol himself carries a bum gene: apoE4, which affects inflammation in the arteries. Unlike MEF2A, it is common; every fourth person has it.
“Heart disease is not a one- or two-gene problem,” says Steven Ellis, a Cleveland Clinic cardiologist who oversees a 10,000-person genetic study known as GeneBank that collects DNA samples from patients who enter hospitals with atherosclerosis. Ellis, like most cardiac researchers, suspects that dozens of genes end up contributing to a predisposition: Some affect arterial integrity, others inflammation (which both causes and exacerbates arterial cracks), and still others the processing of lipids (the fats and cholesterol that turn into plaques). Of the several dozen genes, each may contribute just one percent to a person’s total risk—an amount that may be compounded, or offset, by outside factors like diet. As one doctor told me, any person’s heart attack risk is “50 percent genetic and 50 percent cheeseburger.”
The point of tracking down all these small mutations, Ellis explains, is to create a comprehensive blood test—one that could calculate a person’s genetic susceptibility by adding up the number of risky (and, eventually, beneficial) variables. Combined with other important factors, such as smoking, weight, blood pressure, and cholesterol levels, doctors could decide which patients need aggressive treatment, such as high-dose statins, and which ones are likely to benefit from exercise or other lifestyle changes. Some genes already can predict whose cholesterol level will respond strongly to dietary changes and whose won’t. Assessing risk is crucial, Ellis says, because heart disease is often invisible. In fact, 50 percent of men and 64 percent of women who die of heart disease die suddenly, without experiencing any previous symptoms.
Although standard tests can detect atherosclerosis, they aren’t foolproof. They may reveal plaques, but give no indication whether or not they are life-threatening. Tests like angiography, for example, where doctors inject a dye into the bloodstream and track it with x-rays, can show how much blood is flowing through an artery, but not discern the plaques embedded inside the artery wall—often the culprit in a heart attack.
Researchers have been working to solve this problem with scanners that provide pictures of the arterial wall itself, but it’s a tricky task. Normal cardiac artery walls are about a millimeter thick. Coronary arteries move with every beat of the heart, 70 times a minute. It’s tough to get a clear image of something so small in constant motion.
Difficult, but not impossible. As I walk through the basement of the Cleveland Clinic, I pass a room containing a large, blue, plastic doughnut as tall as I am, with a woman’s legs sticking out of the middle. The doughnut is a computed tomography (CT) scanner, a kind of three-dimensional x-ray machine that’s also used for imaging tumors. The scanner, aided by medications that reduce a patient’s heart rate and an injectable dye that highlights the arteries, can produce startlingly clear pictures.
Scrolling through images on his computer monitor, Mario Garcia, the clinic’s director of cardiac imaging, retrieves one that looks like a black-and-white landscape photographed from a plane, with a single, large river running through it. As Garcia zooms in on the river, a series of white lumps appears on the bank—hard plaques bright with calcium. But there is also a tiny black smudge. “That’s the type we believe causes a heart attack,” he says with satisfaction, pointing to the smudge of soft plaque. “It’s a rare opportunity to see that.”
As compelling as the CT scan is, it’s still an imperfect tool for predicting heart disease. It’s expensive, for one, and the dose of radiation from the x-rays makes it ill suited for use in healthy-patient annual exams. And although it sees arterial plaques, even soft plaques inside arterial walls, it can’t reveal whether those plaques are likely to crack and cause a heart attack.
Until there are tests, genetic or otherwise, that give a clearer measure of risk, everyone would be advised to exercise, watch their diet, and take statins for elevated cholesterol—the same advice doctors gave when the clogged-pipes model of heart disease reigned unchallenged.
At the Cleveland Clinic, cardiologist Stephen Nissen has conducted several studies on statins such as Lipitor, which reduce the amount of LDL (“bad” low-density lipoprotein) cholesterol made by the liver. Nissen is an advocate of lowering cholesterol by any means necessary. Does he take a statin? “You bet!” he says. “I have no intention of dying of the disease I treat.” His LDL level is a paltry 51. Of eight cardiologists I spoke with, all but one were taking the medication. (Some studies now seem to show that lowering even normal cholesterol levels has a protective effect.) HDL (“good” high-density lipoprotein) cholesterol is another story. Nissen calls it the “arterial-wall garbage barge” because of its ability to remove cholesterol from clogged arteries. Not all HDL can do this; some is dysfunctional. But tests have shown that raising the HDL level in genetically engineered lab mice can shrink their arterial plaques.
 A young woman exhales cigarette smoke in Shanghai, China. The People’s Republic of China is both the world’s largest producer and largest consumer of tobacco, which has led to an impending cancer epidemic in the most populous country on Earth.
A young woman exhales cigarette smoke in Shanghai, China. The People’s Republic of China is both the world’s largest producer and largest consumer of tobacco, which has led to an impending cancer epidemic in the most populous country on Earth.