Exercising for Weight Loss (Sex Health Guru)
[media id=33 width=500 height=400]
Physical exercise is any bodily activity that enhances or maintains physical fitness and overall health. It is performed for many different reasons. These include strengthening muscles and the cardiovascular system, honing athletic skills, weight loss or maintenance and for enjoyment. Frequent and regular physical exercise boosts the immune system, and helps prevent the “diseases of affluence” such as heart disease, cardiovascular disease, Type 2 diabetes and obesity. It also improves mental health and helps prevent depression. Childhood obesity is a growing global concern and physical exercise may help decrease the effects of childhood obesity in developed countries.
Types of exercise
Exercises are generally grouped into three types depending on the overall effect they have on the human body:
Flexibility exercises, such as stretching, improve the range of motion of muscles and joints.
Aerobic exercises, such as cycling, swimming, walking, rowing, running, hiking or playing tennis, focus on increasing cardiovascular endurance.
Anaerobic exercises, such as weight training, functional training or sprinting, increase short-term muscle strength.
Categories of physical exercise
Aerobic exercise
Anaerobic exercise
Strength training
Agility training
Sometimes the terms ‘dynamic’ and ‘static’ are used. ‘Dynamic’ exercises such as steady running, tend to produce a lowering of the diastolic blood pressure during exercise, due to the improved blood flow. Conversely, static exercise (such as weight-lifting) can cause the systolic pressure to rise significantly (during the exercise).
Exercise benefits
thumb|right|200px|A common [[elliptical trainer|elliptical training machine.]] Physical exercise is important for maintaining physical fitness and can contribute positively to maintaining a healthy weight, building and maintaining healthy bone density, muscle strength, and joint mobility, promoting physiological well-being, reducing surgical risks, and strengthening the immune system.
Exercise also reduces levels of cortisol, thereby benefiting health. Cortisol is a stress hormone that builds fat in the abdominal region, making weight loss difficult. Cortisol causes many health problems, both physical and mental.
Frequent and regular aerobic exercise has been shown to help prevent or treat serious and life-threatening chronic conditions such as high blood pressure, obesity, heart disease, Type 2 diabetes, insomnia, and depression. Strength training appears to have continuous energy-burning effects that persist for about 24 hours after the training, though they do not offer the same cardiovascular benefits as aerobic exercises do.
Effect on the immune system
Although there have been hundreds of studies on exercise and the immune system, there is little direct evidence on its connection to illness. Epidemiological evidence suggests that moderate exercise appears to have a beneficial effect on the human immune system while extreme exercise appears to impair it, an effect which is modeled in a J curve. Moderate exercise has been associated with a 29% decreased incidence of upper respiratory tract infections (URTI), but studies of marathon runners found that their prolonged high-intensity exercise was associated with an increased risk of an infection, although another study did not find the effect. Immune cell functions are impaired following acute sessions of prolonged, high-intensity exercise, and some studies have found that athletes are at a higher risk for infections. The immune systems of athletes anf nonathletes are generally similar. Athletes may have slightly elevated NK cell count and cytolytic action, but these are unlikely to be clinically significant.
Supplementation with the antioxidants vitamin C and E has been found to decrease the release of interleukin-6 (IL-6), which would be expected to decrease the depression of the immune system. Further, vitamin C supplementation has been associated with lower URTIs in marathon runners. However, the decreased release of IL-6 limits the anti-inflammatory effect of exercse and could limit the positive adaptation effects of exercise.
Biomarkers of inflammation such as C-reactive protein, which are associated with chronic diseases, are reduced in active individuals relative to sedentary individuals, and the positive effects of exercise may be due to its anti-inflammatory effects. The depression in the immune system following acute bouts of exercise may be one of the mechanisms for this anti-inflammatory effect.
Breathing
Active exhalation during physical exercise helps the body to increase its maximum lung capacity. This results in greater efficiency, since the heart has to do less work to oxygenate the muscles, and there is also increased muscular efficiency through greater blood flow. Consciously breathing deeply during aerobic exercise helps this development of the heart and lungs.
Exercising for Weight , Exercising for Weight Health, Exercising for Weight Health Latest, Exercising for Weight Health Information, Exercising for Weight Health information, Exercising for Weight Health Photo,Exercising for Weight Health photo, Exercising for Weight Health Latest, Exercising for Weight Health latest, Exercising for Weight Health Story, Healthy Minnesota Health story, Exercising for Weight Video, Exercising for Weight video, Exercising for Weight Health History, Exercising for Weight Health history, Exercising for Weight over Picture, history, Exercising for Weight Asia, Healthy Minnesota asia, Exercising for Weight Gallery, Exercising for Weight gallery, Exercising for Weight Photo Gallery, Healthy Minnesota photo gallery, Exercising for Weight Picture, Exercising for Weight picture, Exercising for Weight Web, Malaysia Health, web Health, picture, video photo, video surgery, gallery, laparoscopy, virus, flu, drug, video, Health Health, calories, photo, nutrition, health video, symptoms, cancer, medical, beating, diet, organic, blister, exercise, weightloss, surgery, spiritual, Exercising for Weight, tips, operation, bf1,weight, loss, calories, exercise, workout, work ,out, weight, loss, exercises , girls, girl, women, woman, sexy, body, sex, sexual, abs, ass, stomach, fitness, beauty drink, fashion, food, health, home, athletics, medicine, physical, science, video, blog, advice,
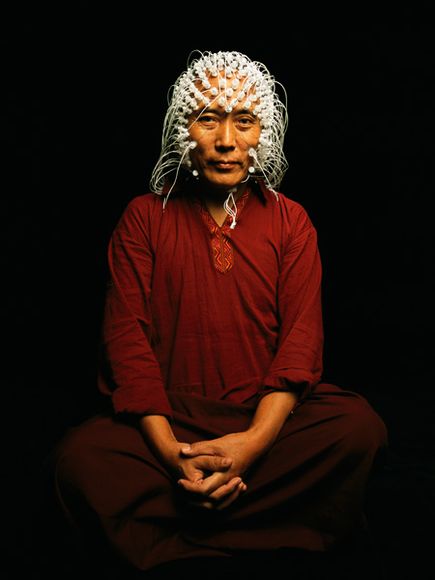
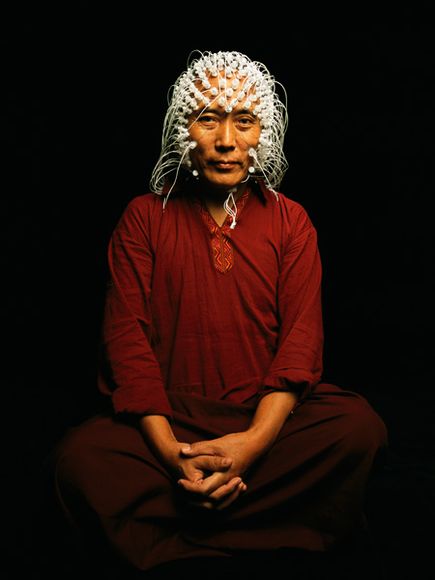 Electrodes measure a Tibetan monk’s brain activity.
Electrodes measure a Tibetan monk’s brain activity.